Math Is Fun Forum
You are not logged in.
- Topics: Active | Unanswered
- Index
- » Science HQ
- » Heparin
Pages: 1
#1 2024-02-22 20:08:39
- Jai Ganesh
- Administrator

- Registered: 2005-06-28
- Posts: 46,281
Heparin
Heparin
Gist
Heparin is obtained from liver, lung, mast cells, and other cells of vertebrates. Heparin is a well-known and commonly used anticoagulant which has antithrombotic properties. Heparin inhibits reactions that lead to the clotting of blood and the formation of fibrin clots both in vitro and in vivo.
Summary
* Heparin injectable solution only comes as a generic drug. It doesn’t have a brand-name version.
* Heparin comes in two forms. One is an injectable solution, which you inject under your skin. The other is a solution that’s injected intravenously (into one of your veins). Only your doctor can give you the intravenous form.
* Heparin injectable solution is a blood thinner that’s used to treat and prevent blood clots.
Important warnings
* Low platelet levels warning. This drug can decrease your platelet levels. This is known as heparin-induced thrombocytopenia (HIT), which can eventually lead to the formation of blood clots in your veins. These clots can form even several weeks after you stop taking heparin. Your doctor will check you for low platelet levels.
* Bleeding risk warning. This drug may cause serious bleeding. This happens because this drug reduces your body’s ability to make your blood clot. Heparin may cause you to bruise more easily. It also may take your body longer to stop bleeding. This can cause death in rare cases. Let your doctor know if you have frequent nosebleeds, unusual bleeding from your gums, periods that are heavier than normal, red or brown urine, or dark or tarry stools. Also let your doctor know if you vomit blood, if your vomit looks like coffee grounds, or if you have headaches, dizziness, or weakness.
What is heparin?
Heparin is a prescription drug. It comes as a self-injectable solution that you inject under your skin. It also comes as a solution that a healthcare provider injects intravenously (into one of your veins). You can only receive the intravenous form in the hospital.
For the injectable solution, you’ll receive your first injection at a hospital. A healthcare provider will show you how to give yourself the injection. You will give yourself the remaining doses at home.
Heparin injectable solution is only available as a generic drug.
Why it’s used
Heparin is a blood thinner that’s used to treat and prevent blood clots. These can include venous thrombosis, pulmonary embolism, and peripheral arterial embolism.
How it works
Heparin belongs to a class of drugs called anticoagulants. A class of drugs is a group of medications that work in a similar way. These drugs are often used to treat similar conditions.
Heparin works by disrupting the formation of blood clots in your veins. It can prevent blood clots from forming, or stop clots that have already formed from getting larger.
Heparin side effects
Heparin injectable solution doesn’t cause drowsiness, but it can cause other side effects.
More common side effects
The more common side effects of this drug include:
* bruising more easily
* bleeding that takes longer to stop
* irritation, pain, redness, or sores at the injection site
* allergic reactions, such as hives, chills, and fever
* increased liver enzymes on liver function test results
If these effects are mild, they may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk to your doctor or pharmacist.
Serious side effects
Serious side effects and their symptoms can include the following:
Severe bleeding. Symptoms can include:
* bruising more easily
* unexpected bleeding or bleeding that lasts a long time, such as:
* unusual bleeding from your gums
* frequent nosebleeds
* periods that are heavier than normal
* pink or brown urine
* dark, tarry stool (may be a sign of bleeding in your stomach)
* severe bleeding or bleeding that you can’t stop
* coughing up blood or blood clots
* vomit that contains blood or looks like coffee grounds
* headaches
* weakness
* dizziness
Serious allergic reactions. Symptoms can include:
* skin tissue death at the injection site
* chills
* fever
* rash and hives
* itching
* burning
* shortness of breath
* swelling of your face, lips, throat, or tongue
Heparin-induced thrombocytopenia. This is low platelet levels caused by heparin use. It can cause new or worsening clots in your blood vessels. These may lead to a stroke or heart attack. Symptoms of new or worsening blood clots can include:
* reddening and swelling of one leg or arm
* coughing up blood
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs affect each person differently, we cannot guarantee that this information includes all possible side effects. This information is not a substitute for medical advice. Always discuss possible side effects with a healthcare provider who knows your medical history.
Heparin may interact with other medications
Heparin injectable solution can interact with other medications, vitamins, or herbs you may be taking. An interaction is when a substance changes the way a drug works. This can be harmful or prevent the drug from working well.
To help avoid interactions, your doctor should manage all of your medications carefully. Be sure to tell your doctor about all medications, vitamins, or herbs you’re taking. To find out how this drug might interact with something else you’re taking, talk to your doctor or pharmacist.
Examples of drugs that can cause interactions with heparin are listed below.
Interactions that can increase your risk of side effects
Taking heparin with certain drugs can increase your risk of bleeding and make you bruise more easily. Examples of these drugs include:
* aspirin
* nonsteroidal anti-inflammatory drugs such as celecoxib, ibuprofen, and naproxen
* antiplatelet drugs such as clopidogrel and dipyridamole
* hydroxychloroquine
* herbal supplements such as ginkgo biloba, fish oil, and garlic
Interactions that can make heparin less effective
When used with heparin, certain drugs can make heparin less effective. Examples of these drugs include:
* digoxin
* tetracycline antibiotics such as doxycycline and minocycline
* nicotine
* nitrates, such as isosorbide, mononitrate, and nitroglycerin
* antihistamines such as diphenhydramine
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs interact differently in each person, we cannot guarantee that this information includes all possible interactions. This information is not a substitute for medical advice. Always speak with your healthcare provider about possible interactions with all prescription drugs, vitamins, herbs and supplements, and over-the-counter drugs that you are taking.
Details
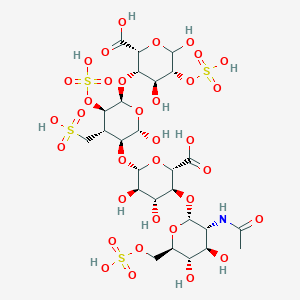
Heparin, also known as unfractionated heparin (UFH), is a medication and naturally occurring glycosaminoglycan. Since heparins depend on the activity of antithrombin, they are considered anticoagulants. Specifically it is also used in the treatment of heart attacks and unstable angina. It is given intravenously or by injection under the skin. Other uses for its anticoagulant properties include inside blood specimen test tubes and kidney dialysis machines.
Common side effects include bleeding, pain at the injection site, and low blood platelets. Serious side effects include heparin-induced thrombocytopenia. Greater care is needed in those with poor kidney function.
Heparin is contraindicated for suspected cases of vaccine-induced pro-thrombotic immune thrombocytopenia (VIPIT) secondary to SARS-CoV-2 vaccination, as heparin may further increase the risk of bleeding in an anti-PF4/heparin complex autoimmune manner, in favor of alternative anticoagulant medications (such as argatroban or danaparoid).
Heparin appears to be relatively safe for use during pregnancy and breastfeeding. Heparin is produced by basophils and mast cells in all mammals.
The discovery of heparin was announced in 1916. It is on the World Health Organization's List of Essential Medicines. A fractionated version of heparin, known as low molecular weight heparin, is also available.
History
Heparin was discovered by Jay McLean and William Henry Howell in 1916, although it did not enter clinical trials until 1935. It was originally isolated from dog liver cells, hence its name (hēpar is Greek for 'liver'; hepar + -in).
McLean was a second-year medical student at Johns Hopkins University, and was working under the guidance of Howell investigating pro-coagulant preparations, when he isolated a fat-soluble phosphatide anticoagulant in canine liver tissue. In 1918, Howell coined the term 'heparin' for this type of fat-soluble anticoagulant. In the early 1920s, Howell isolated a water-soluble polysaccharide anticoagulant, which he also termed 'heparin', although it was different from the previously discovered phosphatide preparations. McLean's work as a surgeon probably changed the focus of the Howell group to look for anticoagulants, which eventually led to the polysaccharide discovery.
In the 1930s, several researchers were investigating heparin. Erik Jorpes at Karolinska Institutet published his research on the structure of heparin in 1935, which made it possible for the Swedish company Vitrum AB to launch the first heparin product for intravenous use in 1936. Between 1933 and 1936, Connaught Medical Research Laboratories, then a part of the University of Toronto, perfected a technique for producing safe, nontoxic heparin that could be administered to patients, in a saline solution. The first human trials of heparin began in May 1935, and, by 1937, it was clear that Connaught's heparin was safe, easily available, and effective as a blood anticoagulant. Prior to 1933, heparin was available in small amounts, was extremely expensive and toxic, and, as a consequence, of no medical value.
Heparin production experienced a break in the 1990s. Until then, heparin was mainly obtained from cattle tissue, which was a by-product of the meat industry, especially in North America. With the rapid spread of BSE, more and more manufacturers abandoned this source of supply. As a result, global heparin production became increasingly concentrated in China, where the substance was now procured from the expanding industry of breeding and slaughtering hog. The dependence of medical care on the meat industry assumed threatening proportions in the wake of the COVID-19 pandemic. In 2020, several studies demonstrated the efficacy of heparin in mitigating severe disease progression, as its anticoagulant effect counteracted the formation of immunothrombosis. However, the availability of heparin on the world market was decreased, because concurrently a renewed swine flu epidemic had reduced significant portions of the Chinese hog population. The situation was further exacerbated by the fact that mass slaughterhouses around the world became corona hotspots themselves and were forced to close temporarily. In less affluent countries, the resulting heparin shortage also led to worsened health care beyond the treatment of covid, for example through the cancellation of cardiac surgeries.
Medical use
Heparin acts as an anticoagulant, preventing the formation of clots and extension of existing clots within the blood. While heparin itself does not break down clots that have already formed (unlike tissue plasminogen activator), it allows the body's natural clot lysis mechanisms to work normally to break down clots that have formed. Heparin is generally used for anticoagulation for the following conditions:
* Acute coronary syndrome, e.g., NSTEMI
* Atrial fibrillation
* Deep-vein thrombosis and pulmonary embolism (both prevention and treatment)
* Other thrombotic states and conditions
* Cardiopulmonary bypass for heart surgery
* ECMO circuit for extracorporeal life support
* Hemofiltration
* Indwelling central or peripheral venous catheters
Heparin and its low-molecular-weight derivatives (e.g., enoxaparin, dalteparin, tinzaparin) are effective in preventing deep vein thromboses and pulmonary emboli in people at risk, but no evidence indicates any one is more effective than the other in preventing mortality.
In angiography, 2 to 5 units/mL of unfractionated heparin saline flush is used to prevent the clotting of blood in guidewires, sheaths, and catheters, thus preventing thrombus from dislodging from these devices into the circulatory system.
Unfractionated heparin is used in hemodialysis. Comparing to low-molecular-weight heparin, unfractionated heparin does not have prolonged anticoagulation action after dialysis, and low cost. However, the short duration of action for heparin would require it to maintain continuous infusion to maintain its action. Meanwhile, unfractionated heparin has higher risk of heparin-induced thrombocytopenia.
Adverse effects
A serious side-effect of heparin is heparin-induced thrombocytopenia (HIT), caused by an immunological reaction that makes platelets a target of immunological response, resulting in the degradation of platelets, which causes thrombocytopenia. This condition is usually reversed on discontinuation, and in general can be avoided with the use of synthetic heparins. Not all patients with heparin antibodies will develop thrombocytopenia. Also, a benign form of thrombocytopenia is associated with early heparin use, which resolves without stopping heparin. Approximately one-third of patients with diagnosed heparin-induced thrombocytopenia will ultimately develop thrombotic complications.
Two non-hemorrhagic side-effects of heparin treatment are known. The first is elevation of serum aminotransferase levels, which has been reported in as many as 80% of patients receiving heparin. This abnormality is not associated with liver dysfunction, and it disappears after the drug is discontinued. The other complication is hyperkalemia, which occurs in 5 to 10% of patients receiving heparin, and is the result of heparin-induced aldosterone suppression. The hyperkalemia can appear within a few days after the onset of heparin therapy. More rarely, the side-effects alopecia and osteoporosis can occur with chronic use.
As with many drugs, overdoses of heparin can be fatal. In September 2006, heparin received worldwide publicity when three prematurely born infants died after they were mistakenly given overdoses of heparin at an Indianapolis hospital.
Contraindications
Heparin is contraindicated in those with risk of bleeding (especially in people with uncontrolled blood pressure, liver disease, and stroke), severe liver disease, or severe hypertension.
Antidote to heparin
Protamine sulfate has been given to counteract the anticoagulant effect of heparin (1 mg per 100 units of heparin that had been given over the past 6 hours). It may be used in those who overdose on heparin or to reverse heparin's effect when it is no longer needed.
Physiological function
Heparin's normal role in the body is unclear. Heparin is usually stored within the secretory granules of mast cells and released only into the vasculature at sites of tissue injury. It has been proposed that, rather than anticoagulation, the main purpose of heparin is defense at such sites against invading bacteria and other foreign materials. In addition, it is observed across a number of widely different species, including some invertebrates that do not have a similar blood coagulation system. It is a highly sulfated glycosaminoglycan. It has the highest negative charge density of any known biological molecule.
Additional Information
Heparin is an anticoagulant drug that is used to prevent blood clots from forming during and after surgery and to treat various heart, lung, and circulatory disorders in which there is an increased risk of blood clot formation. Discovered in 1922 by American physiologist William Henry Howell, heparin is a naturally occurring mixture of mucopolysaccharides that is present in the human body in tissues of the liver and lungs. Most commercial heparin is obtained from cow lungs or pig intestines. Heparin was originally used to prevent the clotting of blood taken for laboratory tests. Its use as a therapy for patients who already have a blood clot in a vein (venous thrombosis) began in the 1940s; low-dose heparin treatment to prevent blood clots from forming in patients who are at high risk for pulmonary embolisms and other clotting disorders was introduced in the early 1970s.
The biological activity of heparin depends on the presence of antithrombin III, a substance in blood plasma that binds and deactivates serum clotting factors. Heparin is poorly absorbed by the intestine, so it must be given intravenously or subcutaneously. Because of its anticlotting effect, the drug creates a significant risk of excessive bleeding, which may be reversed with protamine, a protein that neutralizes heparin’s anticoagulant effect. Other adverse effects of heparin include thrombocytopenia (reduced number of circulating platelets) and hypersensitivity reactions.
It appears to me that if one wants to make progress in mathematics, one should study the masters and not the pupils. - Niels Henrik Abel.
Nothing is better than reading and gaining more and more knowledge - Stephen William Hawking.
Offline
Pages: 1
- Index
- » Science HQ
- » Heparin